A new schedule to get used to now that Evan is down here in Sierra Vista. Thank goodness we live near the hospital and it's on the way to work for us. Since the nursery doesn't have a lot of freezer space, I have to bring in a few bottles every day instead a large bulk amount at UMC. They are fortifying the milk to help him gain weight a bit faster. I think I heard them say he weighs 5lbs. 9oz. now, but I'll check on that.
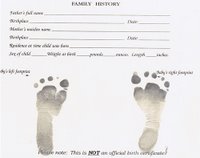
It is funny since to us Evan looks like he's gotten so much bigger, but now that he is beside full-term babies, he still looks so small! The nurses were nice enough to do his feet prints since the prints we had were done very hastily and looked messy. Comparing the earlier feet prints, he has definitely grown. His feet were about 2 inches long at birth, and now they are over 2.5 inches long.
His O2 levels have been steady, so no change to his level. His nasal cannula was half hanging out since the tape holding it on needed replaced. During our evening visit, we asked the nurse (Chrissy) to retape it and it now looks much better. The tape was falling off the past 2 days and we thought someone would take the intiative to change it (um, that didn't happen). Chrissy also suctioned his nose (which we don't think the day shift nurses are doing), and got some nice snot out that was bothering him. He's still eating well, about 60ml/2oz every feeding. They are letting him wake up on his own when he is hungry, but they won't let him go more than 3-4 hours without eating.
If you can tell by my post, I am slightly disappointed in the care Evan is getting in comparision to UMC. Of course it's like comparing apples and oranges to compare the two hospitals. But at UMC, the nurses would make sure his clothes were changed and his bed linens were changed out. I've found that if we don't do it during a visit, it doesn't get done. The nurses also don't practice good inside voices while in the nursery (they talk so loudly all the time). They usually leave the overhead lights on, so tonight we turned one of his fleece blankets into a makeshift tent to cover his face from the light. He's due for a bath tomrrow, so we'll see if the nurses will do it without being reminded.
-----------
SVRHC Charges: $1,822.91
Running Total: $331,790.94
-----------
3 comments:
Jen, make sure they keep his nose clear, especially up in your altitude. They make think his sats are dropping and really all it is, is clogged nares. If they are only using a blue blub syringe, it is not enough sometimes. There is a "nasal aspirator" that connnects to the suction that is better if they have it. It has a white bulb like end. We called it a boogie sucker. That combined with some saline and life is good.
Nursery nurses usually only do healthy babies, so the care will be apples to oranges as you said. They will most likely be working short staffed (my experience the last 3 years back in adult health care)and you may have to ask for things to get done unfortunately or do it yourself. It will be good bonding time for you to bath and change his clothes since he doesn't have as many wires. Just tell them that you would like to do it if they could bring you the things you need and help you. The hospital environment and staff can be intimidating and make one naturally feel apprehensive. You guys have not been able to hold Evan and do the usual things because of the ICU, now you can. Tell the nurses you just need some guidance and transition from the ICU setting.
Even if he has to go home on O2, lots of babies do, you will want him out of there as soon as possible. They can send him home on an apnea monitor, plus the O2 and concentrator/portable tanks for trips to the doctor.
At this point, I think you guys will almost have to step in to do more things, or it won't get done, frustration will rise. Learn how to retape the cannula with one of the nurses or RT (it usually takes two, unless you are fast). Learn how to change the pulse oximeter and have them leave an extra one or two at the bedside. Those really should be changed every day to ensure accuracy, although most nurses won't change them until they aren't sticking anymore.
Anything that is stressing you out when you go in, try to turn it around, take control and figure out if it something you can do. That way you guys will get Evan out of there sooner. As soon as you can "room in", then you need to in order to watch what is going on.
So, just some hints from the old nurse........ It sounds like it won't be much longer before he can go home. Remember, the boogies need sucked out, then you will have a good oximetry reading.
Sis
Jen
I hope things go better for you @ SV. I have still been praying for Evan. I know he will be coming home very soon. This may be the last time I leave a comment as this is my be my last day of work. I was measuring 40wks @ my 36wk checkup. I am having an u/s on Tuesday 5th, and will know more then, they my induce me..Thank you for allowing me in some small way (praying) to be apart of your life. I really care about Evan and you guys although I will never know or meet you..He is doing sooo well and is sooo cute, you guys will be home before you know it..If I get to a computer I will try to check in with you later...Lots of love from my family to yours....
Lynette & Bryan
edd 9.25.06(Nathan)
ds 3.28.05(Brandon)
dd 1.12.96(Melody)
ds 11.30.93(Dalton)
Hi Jen,
Glad to hear he is doing well. He is really adorable!!! Miss you guys.
Love,
Kim and Sue
Post a Comment